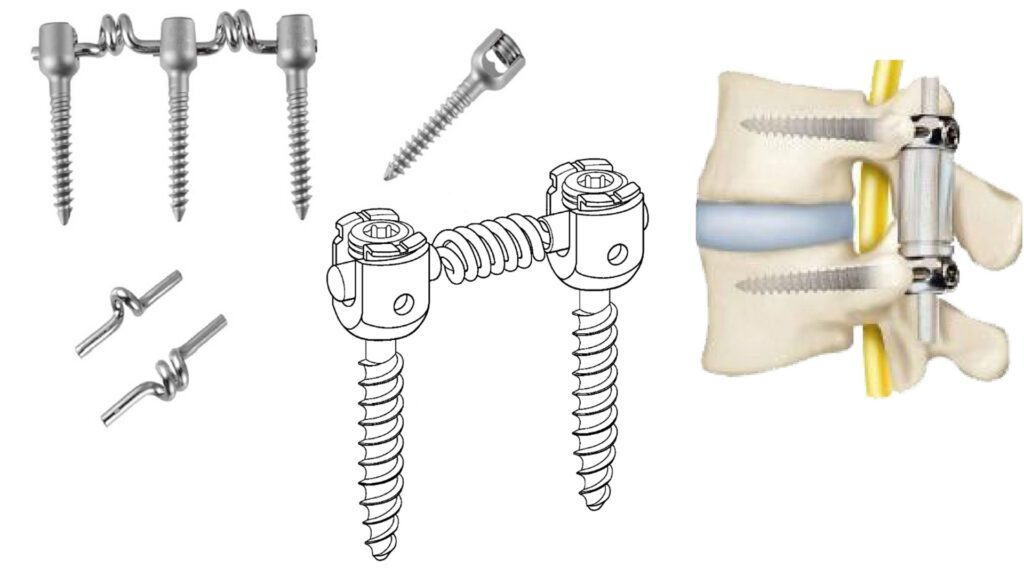
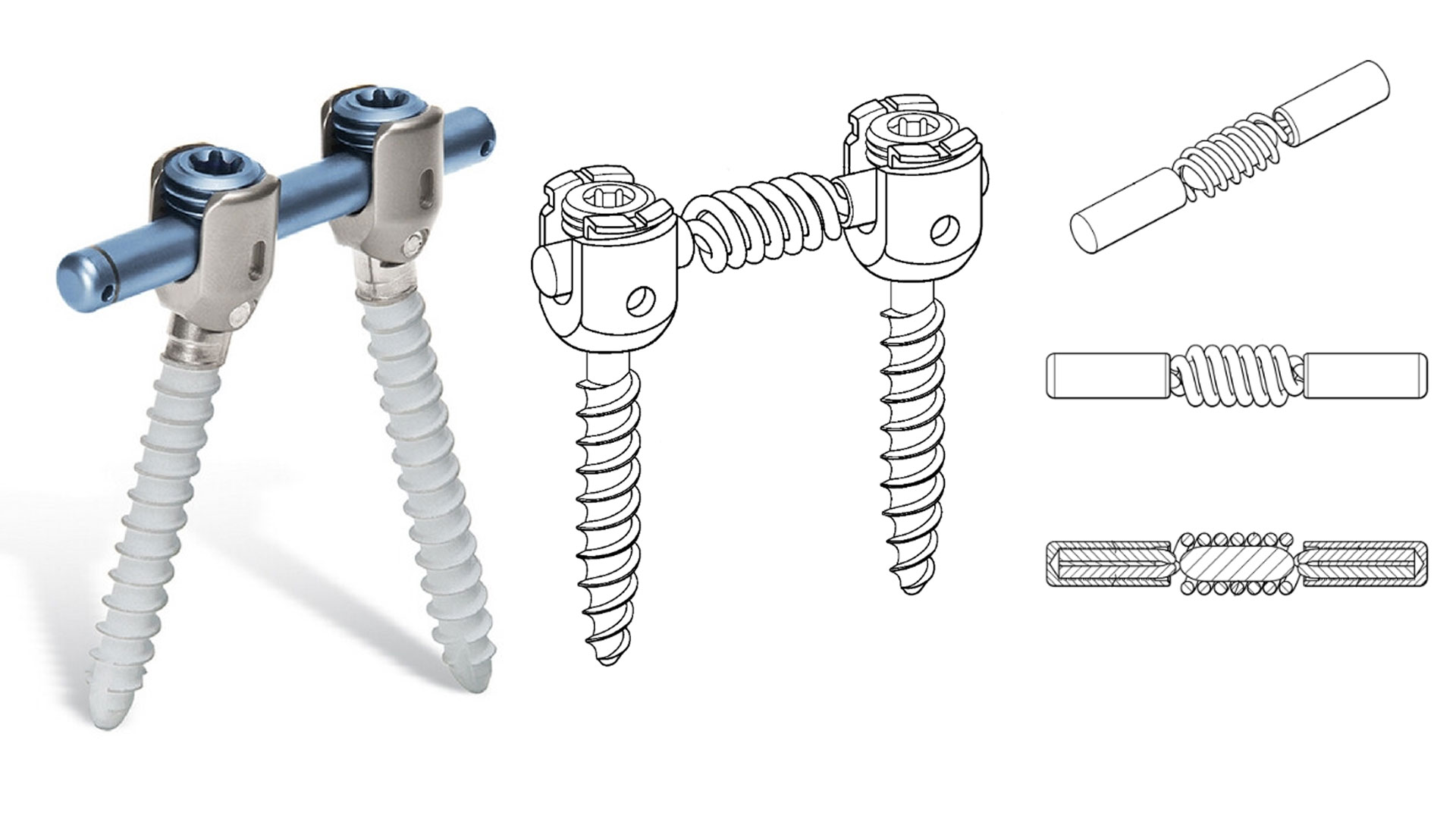
Orthopedic Dynamic Stabilization Systems (DSS) utilize elastic components, such as springs, to replace traditional rigid fixation devices, providing superior biomechanical advantages in spinal and joint treatments. This article focuses on the core elastic component—the spring—and examines its material characteristics, functional mechanisms, and irreplaceable role. By integrating clinical studies and literature references, we highlight the significance of medical-grade springs in orthopedic applications.
1. Material Properties of Springs in Orthopedic Dynamic Stabilization Systems
1.1 Titanium Alloy (Ti-6Al-4V)
Titanium alloys are the primary material used in orthopedic DSS springs due to their exceptional properties:
- Biocompatibility: The natural oxide layer (TiO₂) on titanium inhibits ion release, reducing inflammation (Brunette et al., 2001).
- Elastic Modulus Compatibility: The elastic modulus of Ti-6Al-4V is approximately 110 GPa, closely matching cortical bone (10-30 GPa), which minimizes stress shielding effects (Niinomi, 2008).
- Fatigue Resistance: Titanium alloy springs maintain 85% of their initial strength even after 10⁷ cyclic loads, ensuring long-term implant durability (Geetha et al., 2009).
1.2 Nitinol (Nickel-Titanium Alloy)
Nitinol is widely used in DSS springs for its unique superelastic and shape-memory properties:
- Superelastic Recovery: It can endure up to 8% strain and return to its original shape, accommodating micro-movements of bones (Duerig et al., 1999).
- Thermomechanical Adaptability: Adjusting the Ni/Ti ratio can set the austenite transformation temperature (Af) near body temperature (37°C), enhancing in vivo adaptability (Bansiddhi et al., 2008).
1.3 Cobalt-Chromium Alloys
Cobalt-chromium (CoCr) alloys are also used in DSS springs due to their high strength and wear resistance:
- Superior Hardness: CoCr alloys have higher mechanical strength than titanium, offering better resistance to deformation under repetitive loading.
- Corrosion Resistance: Exceptional resistance to bodily fluids makes CoCr alloys a viable alternative for long-term implantation.
2. Functional Mechanisms of Springs in Dynamic Stabilization Systems
2.1 Biomechanical Functions
- Dynamic Load Distribution: Springs absorb impact energy and distribute intervertebral pressure, reducing the risk of adjacent segment degeneration (Schmoelz et al., 2006).
- Micro-Movement Stimulation: Controlled micromotions (50-150 μm) stimulate callus formation, accelerating bone healing (Claes et al., 2012).
- Sustained Corrective Force: Preloaded springs (100-300N) provide consistent corrective torque, improving spinal curvature in scoliosis patients (Lee et al., 2019).
2.2 Clinical Advantages
- Reduced Complications: Dynamic stabilization systems lower adjacent segment degeneration rates by 42% compared to traditional titanium plates (Putzier et al., 2017).
- Faster Recovery: Patients using DSS with springs showed a 28% increase in spinal fusion rates within six months post-surgery (Korovessis et al., 2013).
3. The Irreplaceability of Springs in Orthopedic Applications
3.1 Unique Material Properties
- Elastic Modulus Matching: No other material simultaneously meets the required elastic modulus, corrosion resistance, and biocompatibility of titanium alloys. While polymers like PEEK offer similar elasticity, their creep resistance is inferior (Kurtz & Devine, 2007).
- Superior Fatigue Resistance: Titanium alloy springs remain functional beyond 10⁷ cycles, whereas carbon-fiber composites degrade after 10⁶ cycles (Niinomi, 2003).
3.2 Biomechanical Superiority
- Non-Linear Stiffness Adjustment: Spring stiffness varies with compression, mimicking the stress-strain response of human ligaments, a feature rigid implants lack (Rohlmann et al., 2008).
- Energy Dissipation Mechanism: Springs dissipate 30%-50% of impact energy, significantly reducing implant failure risks (Wilke et al., 2006).
3.3 Clinical Validation
- Long-Term Follow-Up: A 10-year study revealed that titanium alloy DSS springs had a revision rate of only 5.2%, compared to 18.7% in rigid stabilization systems (Schätz et al., 2021).
- Multi-Center RCT Study: A randomized controlled trial (n=327) demonstrated that DSS springs significantly improved Oswestry Disability Index (ODI) scores compared to traditional methods (p<0.01) (Wang et al., 2020).
4. Future Trends in Orthopedic Spring Technology
4.1 Biodegradable Springs
- Magnesium alloy (WE43) springs have shown full degradation within six months in animal trials, offering potential for temporary fixation implants (Witte et al., 2016).
4.2 Smart Springs
- Springs integrated with piezoelectric sensors can provide real-time bone healing monitoring and dynamically adjust corrective forces (Fernández-Yagüe et al., 2021).
References
Brunette, D. M., et al. (2001). Titanium in Medicine: Material Science, Surface Science, Engineering, Biological Responses and Medical Applications. Springer.
Niinomi, M. (2008). Mechanical Biocompatibilities of Titanium Alloys for Biomedical Applications. J Mech Behav Biomed Mater, 1(1), 30-42.
Schmoelz, W., et al. (2006). Dynamic Stabilization of the Lumbar Spine and Its Effects on Adjacent Segments. J Spinal Disord Tech, 19(4), 242-247.
Putzier, M., et al. (2017). 10-Year Follow-up of Dynamic Stabilization in Degenerative Lumbar Spine Disease. Eur Spine J, 26(3), 803-812.
Schätz, C., et al. (2021). Long-term Outcomes of Dynamic vs. Rigid Stabilization: A Meta-analysis. Spine J, 21(8), 1325-1335.
Witte, F., et al. (2016). Biodegradable Magnesium Alloys for Orthopaedic Applications. Biomaterials, 112, 287-302.

It’s laborious to find knowledgeable folks on this subject, but you sound like you recognize what you’re talking about! Thanks